Dogs are usually very important members of our families! This leads us to think of them as like us in so many ways. But do we know their oral health is as important for them as it is for us?
The fact is, that problems related to teeth and gums can dramatically decrease our pet’s quality of life, as well as lead to expensive and unnecessary dentistry costs.
Are oral health issues in dogs really that common though?
- Yes! By just two years of age, 70% of cats and 80% of dogs have some form of periodontal disease (gum disease), with small and toy breed dogs,who are increasing in popularity, being particularly susceptible.
- One study of North American pets demonstrated a 20% incidence of calculus and or gingivitis shown in dogs across all age categories. 1
- Another study showed that 82% of dogs aged 6 to 8 years and 96% in dogs aged between 12-14 years, had periodontitis. 2
Dental disease in dogs, is therefore, very common. But the good news is, in many cases, we can reduce the incidence of disease in our dogs with monitoring and prevention - just like we do when we vaccinate them or treat them with anti-parasitics.
While it may seem a hassle to make teeth care part of the daily routine – oh if only they could brush their own teeth! – it’s just as important as walking them, keeping their vaccinations up to date and giving them a great diet. (Hello bestie.)
A daily dental care routine can help prevent dental health problems in dogs. However, given that only about 2% of dog parentspractise daily tooth brushing, we thought we’d help with The Smooch. This health booster, with cranberry, green tea & citrus polyphenols in vet-formulated daily doses, helps reduce oral bacteria, and freshen their breath.
That said, sometimes a dog with an excellent oral healthcare routine can succumb to dental disease as a result of a systemic illness, their age, weight, breed and genetics.
In this article, we will cover:
- The importance of good oral health in dogs
- How to estimate the condition of your dog’s mouth
- Signs that your dog may need a vet to treat their teeth or gums and what this can involve
- Factors that affect the condition of a dog's teeth and the progression of dental disease
- Information about how to keep your dog's mouth in good condition
Knowing what to do and actually doing it, are two key factors leading to poor oral health of dogs and both are things that we as pet parents have the ability to control.
So, let’s get our teeth stuck in!
What does good oral health and healthy teeth look like in dogs?
Besides eating, whether your dog uses their mouth to carry their favourite toys around or they’re the chatty type who love to woof with their friends, a happy dog has a healthy mouth.
The consequences of poor dental hygiene and secondary health problems don’t appear overnight. It’s important to note that it can be resolved – up to the stage of severe gingivitis.
Dr Tom Lonsdale, an Australian veterinary surgeon, dental disease expert and proponent of raw meaty bones for dogs, describes five grades of periodontal disease 3:
- ‘Healthy’ (sometimes known as grade 0) – the outline between the tooth and gum is well defined and pale pink in colour, there is no smell present.
- ‘Grade I’ – ‘Marginal gingivitis’. The edges of the gum surrounding the tooth are inflamed and there is now a smell present.
- ‘Grade II’ – ‘Moderate gingivitis’. In addition to inflammation there is swelling of the ‘margins’ of the gums.
- ‘Grade III’ – ‘Severe gingivitis’. With more swelling and changes in colour of the gum ‘margins’ and ‘beginning pocket formation beyond normal 1 to 3mm depth’ – up to this stage of gingivitis, the condition can be reversible.
- ‘Grade IV’ – ‘Moderate periodontitis’. With ‘severe inflammation, deep pocket formation, beginning bone loss’ with loss of attachment to the gum and ‘tooth mobility and tooth loss’. Periodontitis is not reversible, it is only possible to slow down its progression.
- ‘Grade V’ – ‘Severe periodontitis. Advanced epithelial attachment loss, advanced bone loss, tooth mobility and tooth loss.’ 3
It is also important to note that the above can be complicated by ‘foreign body lodgement’, ‘trauma’ and ‘teething’.3
Chronic gingivitis and periodontitis as a result of inadequate oral care and progression of the above grades, can lead to painful conditions in the oral cavity such as:
- Tooth rotting
- Jaw fractures
- Tooth abscesses
-
Gingival recession
(exposure of a tooth’s root due to destruction of gums secondary to disease, grade 3) 4
- Bone loss (grade 4)
A great illustration that shows a similar progression is shown here.

Source: https://smile4pet.com/stages-of-periodontal-disease/
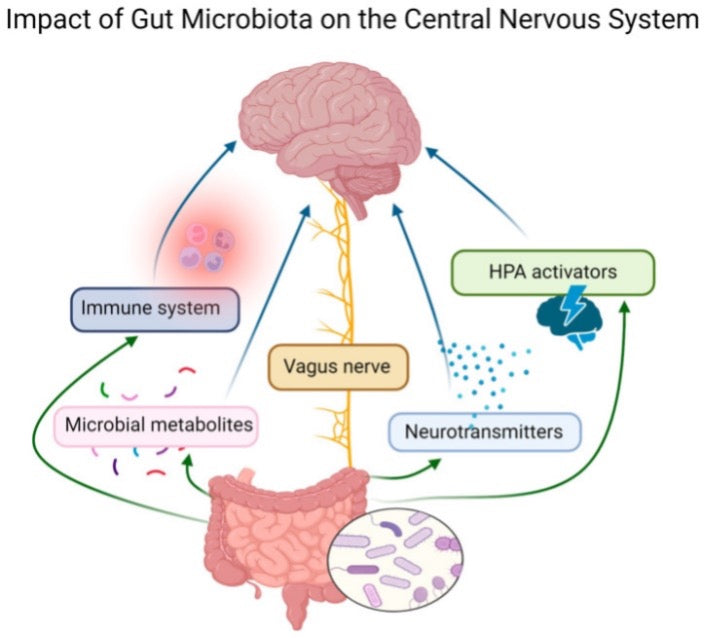
Unfortunately, the problem does not always start and end in the mouth. The above conditions can lead to the translocation of bacteria systemically via the blood, and disease in other organ systems.
Studies in humans have shown links between inflammatory mediators present in periodontitis and other health problems such as cardiovascular disease, coronary heart disease, atherosclerosis. 5
’Significant associations’ have also been proven ‘between the severity of periodontal disease and the subsequent risk of cardiovascular-related conditions’ 6in dogs. The ‘positive relationship’ ‘between periodontal disease and cardiac disease’ 7is something that we, as owners, have the possibility to influence.
For pet parents, a dog with an unhealthy mouth can be unpleasant to be around and lead to financial strain following expensive veterinary procedures.
Often a dog with dental problems can have very bad breath and can be the initial reason why owners seek veterinary advice.
If disease is already developed then significant costs for owners can occur in the forms of surgeries and or medication.
How to estimate the condition of your dog’s mouth and oral health
Oral health assessment in dogs begins at home.Signs we may observe in dogs suffering from dental disease include:
- Bad breath
- Difficulty chewing food
- Dropping food from the mouth
- Secondary weight loss
- Tooth loss
These signs can be seen without even opening the mouth and taking a look inside. However, some dogs will tolerate you opening their mouth to inspect their teeth and gums. If they will, look for these signs:
- Gum bleeding
- Calculus or tartar on the teeth
- Loose, broken or missing teeth
- Change in colour of teeth indicating decay
- Swelling or painful areas on the gums indicating inflammation and affecting your dog’s behaviour and ability to eat.
By the way, we use the term ‘plaque’ in both human and dog oral health. It refers to the substance left on teeth after a meal. ‘Tartar’ or ‘calculus’ are the terms used when, over time, plaque combines with saliva and hardens to a brown substance on teeth, which can accumulate both above and below the teeth.
‘First, tartar forms a rough surface serving as a solace for bacteria to grow and multiply in the mouth. Bacteria can cause inflammation of the gums (gingivitis) which often results in painful bleeding……As tartar builds up along the gum line, it pushes the gums away from the roots of the teeth. As their gums recede, they expose the sensitive, enamel-free part of the tooth which causes sensitivity and pain.’ Jan Bellows, DVM, Dipl. AVDC, ABVP 8
In addition, not all owners know that our dogs are also susceptible to caries.
‘Caries results from bacterial decay of the tooth structure brought about by the release of acids from oral bacteria fermenting carbohydrates on the tooth surface.’ Fraser A. Hale 9
So, how do you know if it’s time for a trip to the vet outside of your routine visit? If you see any of the signs above then it’s probably worth checking in…
What does veterinary dentistry for dogs involve?
During the initial consultation your vet will perform an examination of the oral cavity, head and neck but also assess the general condition of your dog by performing a physical exam.
They will also ask you for information regarding your dog’s medical history. It is possible that a change in physical condition can link to dental disease. Painful teeth and gums can cause your dog to eat less and lose weight.
Before opening the mouth, the vet will observe and palpate any changes seen from outside your dog’s mouth. They will record all observations in a dental chart.
Your vet will then look inside the mouth and may ask you to restrain your dog. They will examine the lips, mucosa, palate, teeth and tongue and may use an instrument to assist them.
If necessary, they may then decide to anaesthetise your dog. This will enable them to perform even more thorough checking manually and with an x-ray and then begin treatment accordingly.
The prospect of anaesthetising your dog may sound scary, but it will allow the vet to perform a more thorough examination and minimise the stress involved for your dog.
Vets are responsible for assessing whether your pet is a suitable candidate to undergo anaesthesia beforehand. This assessment helps to minimise any risks
It is important to ask your vet regarding any questions you may have regarding anaesthesia or the condition of your dog’s teeth.
Dentistry procedures they may perform during anaesthesia can include:
- Taking x-rays
- Teeth removal
- Periodontal probing
- Irrigation (washing)
- Grinding and polishing to remove calculus 10
After the examination and procedure, your vet will discuss the findings with you and any next steps in terms of any treatment, or prophylactic measures.
What factors contribute to oral health issues and how can you help?
‘Dietary strategies to promote dental health have been established and can be useful additions to a complete home oral care regimen’ Jennifer Larsen, DVM, PhD, DACVN, University of California, Davis 4
Our dog’s oral health is the result of many factors both under and above our control as owners. For example:
- The diet we feed them has a huge impact by its possibility to facilitate the prevention of calculus build up. Feeding more abrasive food acts as a mechanism to brush teeth.
- Feeding nutraceutical formulations like the anti-bacterial and antioxidant blend, in bestie The Smooch also helps decrease bad breath and improve oral health.
- ‘Fermentable carbohydrates are recognised as a necessary cause of dental caries’ 11. Feeding a diet high in fermentable carbohydrates can have a negative effect on the condition of your dog’s teeth as they ‘provide substrate for the actions of oral bacteria.’ 12
- Studies have proven ‘daily tooth brushing in dogs to be the single most effective method of reducing plaque accumulation and optimise dogs’ oral health’ 13when compared to the use of dental chews or a prescription dental diet formulated food.
- Vets recommend brushing your dog’s teeth with a special dog toothbrush and toothpaste once per day if they will tolerate it. Be sure only to use dog specific products for this as the components of human products (especially toothpaste) are not safe for use in dogs. Be aware that brushing will not remove calculus, it only removes plaque. Also,
- If your dog does not allow you to brush their teeth, there are a variety of foods and treats aimed to assist with mechanical abrasion (brushing) of teeth. However, many vets advise against the use of hard treats (such as bones) in mechanical cleaning of teeth. 15
- Vets also recommend that dogs undergo professional teeth cleaning once a year, in addition to regular brushing. They suggest puppies of small to medium dogs undergo their first routine dental check before the first year of age and for larger dogs by the second year of age and then every 6 months thereafter. 15
Oral health in dogs can also be affected by factors outside of owners or veterinarians’ control.
- Brachycephalic dogs (dogs with a short head such as pugs and bulldogs) are more prone to overcrowding 10which can lead to an increased risk of dental disease. 14
- Developmental diseases and defects in puppies can also provoke dental disease in later life. Older dogs are also more likely to suffer from dental disease.
The first step in maintaining good oral health for our dogs is to be informed and to act upon such information. So the good news is, after reading this article you’re well on the way!!
Charlotte Francesca Stiles
Charlotte is a 5th-year veterinary medicine student at the University of Zagreb, Faculty of Veterinary Medicine. She is a volunteer at her university's obstetrical clinic, equine clinic, an editor of her university's scientific journal, and dog mum to 12-year-old Chiki.
Charlotte is particularly interested in wildlife medicine and research and hopes that her current extra-curricular work as a student in this area will help her achieve a scientific career after graduation.
References
1Lund, E. M., Armstrong, P. J., Kirk, C. A., Kolar, L. M., & Klausnor, J. S. (1999). Health status and population characteristics of dogs and cats examined at private veterinary practices in the United States. Journal-American Veterinary Medical Association, 214, 1336-1341.
2Hamp, S.-E., Olsson, S.-E., Farsø-Madsen, K., Viklands, P. and Fornell, J. (1984), A MACROSCOPIC AND RADIOLOGIC INVESTIGATION OF DENTAL DISEASES OF THE DOG. Veterinary Radiology, 25: 86-92. https://doi.org/10.1111/j.1740-8261.1984.tb01916.x
3Londsdale, T. ‘Pandemic of periodontal disease a malodorous condition’ Presentation to Sydney metropolitan practitironers branc Australian veterinary association, 20th August 1992
4 Jennifer Larsen, (2010), Compendium: Continuing Education for Veterinarians, ‘Oral products and dental disease’ https://www.researchgate.net/publication/47500936_Oral_products_and_dental_disease
5Cullinan, M., Ford, P. and Seymour, G. (2009), Periodontal disease and systemic health: current status. Australian Dental Journal, 54: S62-S69. https://doi.org/10.1111/j.1834-7819.2009.01144.x
6 Lawrence T. Glickman VMD, DrPH1, Nita W. Glickman MPH, PhD2, George E. Moore DVM, PhD, DACVPM, DACVIM3, Gary S. Goldstein DVM, DAVDC4, and Hugh B. Lewis DVM, DACVP5 5 ‘Evaluation of the risk of endocarditis and other cardiovascular events on the basis of the severity of periodontal disease in dogs’ https://doi.org/10.2460/javma.234.4.486,Volume 234: Issue 4
7José Diogo Pereira dos Santos, Eva Cunha, Telmo Nunes, Luís Tavares, Manuela Oliveira,
‘Relation between periodontal disease and systemic diseases in dogs’,Research in Veterinary Science,Volume 125,
8Jan Bellows, (2009) Plaque and Tartar Prevention in Dogs, https://vcacanada.com/know-your-pet/tartar-prevention-in-dogs
9Hale F. A. (2009). Dental caries in the dog. The Canadian veterinary journal = La revue veterinaire canadienne, 50(12), 1301–1304., https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2777300/
10 https://www.rvc.ac.uk/review/dentistry/Shared_Media/pdfs/perio_print.pdf
11P. Hujoel D, Dietary Carbohydrates and Dental-Systemic Diseases, DOI:10.1177/0022034509337700 J DENT RES 2009; 88; 490
12Sugars and dental caries1–4 Riva Touger-Decker and Cor van Loveren
13Allan, R.M., Adams, V.J. and Johnston, N.W. (2019), Prospective randomised blinded clinical trial assessing effectiveness of three dental plaque control methods in dogs. J Small Anim Pract, 60: 212-217. https://doi.org/10.1111/jsap.12964
14O'Neill, D.G., Mitchell, C.E., Humphrey, J., Church, D.B., Brodbelt, D.C. and Pegram, C. (2021), Epidemiology of periodontal disease in dogs in the UK primary-care veterinary setting. J Small Anim Pract, 62: 1051-1061. https://doi.org/10.1111/jsap.13405
15https://www.aaha.org/globalassets/02-guidelines/dental/aaha_dental_guidelines.pdf